Running a medical practice involves a lot of moving parts, and one of the most important—yet often overlooked—areas is the billing process. Medical billing can be complex, time-consuming, and prone to mistakes, especially with the ever-changing insurance rules and coding systems. For many healthcare providers, outsourcing medical billing is a way to relieve that burden. By letting experts handle billing, you can improve your cash flow, reduce errors, and focus more on patient care.
In this blog, we’ll break down the benefits of outsourcing medical billing, how the U.S. medical billing system works, and why ClearPath Medical Billing LLC is the best partner for healthcare providers looking to streamline their billing operations.
What’s the US Medical Billing System All About?
Before diving into why outsourcing is beneficial, it’s important to understand how the U.S. medical billing system functions. Medical billing is a process that ensures healthcare providers get paid for their services. Here’s how it works in a nutshell:
- Patient Visits the Healthcare Provider: The patient receives care from a doctor, specialist, or hospital.
- Healthcare Provider Documents Services: The provider records details of the visit, including diagnoses, treatments, and procedures, using specific codes (like ICD-10, CPT, and HCPCS codes).
- Medical Bill Creation: These codes are used to create a medical claim, which is sent to the insurance company or payer for reimbursement.
- Claim Submission: The claim is sent electronically or on paper to the insurance company for review.
- Claim Review (Adjudication): The insurance company reviews the claim and decides how much to pay. They either approve or deny it based on their rules.
- Payment: If approved, the insurance company sends payment to the healthcare provider, and the patient might need to pay some amount out-of-pocket (like a copay or deductible).
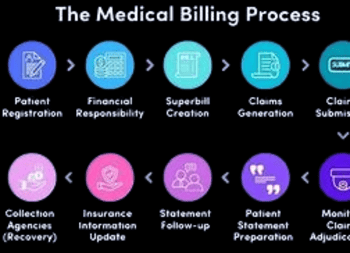
While the process seems straightforward, it’s not always easy to handle. Billing can get complicated fast, especially with the huge number of claims that need to be processed. That’s why many practices choose to outsource it.
Challenges of In-House Medical Billing

Managing medical billing internally comes with a set of challenges that can be overwhelming, including:
- Complex Codes and Regulations: The codes used for medical procedures, diagnoses, and services can be confusing and change frequently. Providers must stay up to date with the latest codes and regulations.
- Time-Consuming: Billing isn’t just about submitting claims—it’s about making sure everything is correct, following up on denied claims, and keeping track of all the details. This takes up a lot of time and can distract from patient care.
- Hiring and Retaining Staff: You need skilled staff to handle medical billing, but hiring and maintaining a qualified team can be expensive and time-consuming. Plus, it can be hard to keep up with the constant changes in billing rules and insurance policies.
- Risk of Errors and Denied Claims: Mistakes in coding, missing details, or late submissions can lead to claim denials. These denials mean delayed payments, which can hurt your practice’s financial health.
- Cash Flow Problems: Slow reimbursement cycles can lead to cash flow issues. When payments from insurance companies take too long to come through, it can impact your ability to cover operating expenses.
The Many Benefits of Outsourcing Medical Billing
Outsourcing medical billing offers a variety of benefits that can improve your practice’s bottom line and help you focus more on your patients. Here’s why many healthcare providers make the switch:
Save on Costs
Outsourcing medical billing can save you money by cutting down on staffing costs and overhead. Instead of hiring an in-house team, paying salaries, training, and benefits, you pay a set fee for billing services. This way, you know exactly what to expect.
2. Fewer Errors and Denials
Billing professionals are experts in their field. They know the ins and outs of medical codes, payer requirements, and regulations. This expertise reduces the chances of making errors, which means fewer denied claims and faster payments.
3. Faster Payments and Better Cash Flow
Outsourcing medical billing means claims are processed and followed up on quickly. Because professional billing companies specialize in getting claims paid, providers see faster reimbursements, which helps maintain smooth cash flow.
4. Focus on Patient Care
Billing can be incredibly distracting for healthcare providers. When you outsource, you can spend more time with your patients instead of managing claims, paperwork, and follow-ups. This helps improve patient care and overall satisfaction.
5. Stay Compliant with Regulations
The healthcare industry is full of regulations—like HIPAA, CMS rules, and payer-specific policies—that change regularly. Billing experts are always up to date with the latest rules, making sure your practice stays compliant and avoids costly penalties.
6. Access to Expert Knowledge
By outsourcing, you get access to a team of billing experts who have extensive knowledge of coding, claim management, and the latest insurance industry trends. They’ll know how to handle even the most complex cases.
7. Scalability
Outsourcing allows your practice to scale your billing services up or down as needed. Whether you’re a solo practitioner or part of a larger healthcare system, a medical billing company can adjust to meet your needs.
8. Use of Advanced Technology
Billing companies invest in the latest software and technology, which streamlines processes and improves accuracy. Instead of spending money on billing systems and infrastructure, you get access to these tools as part of your service.
9. Lower Administrative Workload
Medical billing involves a lot of paperwork and administration. When you outsource this task, you reduce your team’s administrative workload and free up resources to focus on more important tasks.
Why Choose ClearPath Medical Billing LLC?
Outsourcing to the right medical billing company is crucial. That’s where ClearPath Medical Billing LLC comes in. Here’s why healthcare providers choose ClearPath as their trusted billing partner:
1.Trusted and Reliable
ClearPath Medical Billing LLC has built a solid reputation over the years for being a trusted and reliable billing partner. They’ve proven time and again that they can handle your billing needs accurately and efficiently, so you can focus on what really matters—your patients.
2. Expert Team of Professionals
ClearPath is home to a team of highly skilled billing professionals. They understand the complexities of the U.S. medical billing system and are well-versed in coding, claims processing, and payer requirements. Their experience helps ensure that your claims are submitted correctly and get paid faster.
3. Low-Cost Solutions—Only 5% Fee
One of the best parts about ClearPath is their incredibly competitive pricing. They offer billing services for just 5%, which is an excellent value for the quality of service they provide. Healthcare providers can save money while still getting top-notch billing solutions.
4. Full Range of Services
ClearPath doesn’t just do billing. They offer a full range of services that help streamline your revenue cycle, including:
- Credentialing: Helping you get properly credentialed with insurance companies so you get paid on time.
- Benefits Verification: Ensuring patients’ insurance benefits are verified so you don’t face surprise claim denials.
- Claim Denial Management: Taking care of denied claims and making sure they’re appealed and processed correctly.
- Patient Help Desk: Assisting patients with billing questions and concerns to improve their experience and communication.
- Account Receivable (AR) Services: Managing unpaid claims and ensuring timely payments from insurance companies.
5. Commitment to Accuracy and Compliance
ClearPath is all about accuracy. They work diligently to make sure every claim is submitted correctly, reducing errors and denials. They also stay on top of all regulations and industry standards to ensure your practice stays compliant.
6. Faster Payments and Improved Cash Flow
Thanks to their streamlined process, ClearPath helps providers get paid faster. Their team’s focus on accuracy and timely submission means fewer delays and better cash flow for your practice.
7. Scalability and Flexibility
Whether you’re a solo practitioner or part of a larger group, ClearPath can scale their services to meet your practice’s needs. They offer flexible billing solutions that grow with you.
Range of Services
1. Credentialing Services
Credentialing is the process of verifying the qualifications, experience, and professional history of healthcare providers so they can join insurance networks. Insurance companies need to ensure that healthcare providers meet specific standards before they’re reimbursed for services rendered.
ClearPath Medical Billing LLC helps healthcare providers navigate the credentialing process, which can be quite complicated and time-consuming. They ensure that all necessary paperwork and documentation are completed correctly and submitted to the right insurance companies. By doing this, they help providers get enrolled in insurance networks quickly, so they can start accepting insurance and getting paid without unnecessary delays.
2. Benefits Verification
Before providing medical services, it’s important for healthcare providers to confirm whether the patient’s insurance covers those services, and if so, what’s included. This process is known as benefits verification. It involves confirming details like:
- Whether the patient’s insurance policy is active
- The types of medical services covered
- Any deductibles, copays, or coinsurance the patient may owe
- The insurance company’s billing requirements
ClearPath Medical Billing LLC helps ensure that this process is handled efficiently. By verifying the patient’s benefits ahead of time, healthcare providers can avoid surprises, like claim denials due to coverage issues. It also helps the provider understand how much of the cost will be covered by insurance and how much the patient will need to pay out of pocket, improving transparency and communication with patients.
3. Claim Denial Management
In the world of medical billing, claim denials are a common issue. When an insurance company denies a claim, it means the provider won’t get paid unless the issue is addressed. Denials can happen for many reasons, such as incorrect coding, missing information, or billing issues.
ClearPath Medical Billing LLC handles claim denials expertly by thoroughly reviewing denied claims and determining the cause of the denial. Once the issue is identified, they take the necessary steps to correct the problem, whether that’s fixing coding errors, submitting additional documentation, or appealing the decision to the insurance company.
Their experienced team ensures that claims are resubmitted or appealed in a timely and accurate manner, increasing the likelihood that providers will eventually get paid. This process minimizes the financial impact of denials and helps maintain consistent revenue flow for healthcare practices.
4. Patient Help Desk
Dealing with medical bills can sometimes be confusing for patients, especially when they’re unsure about what they owe or why they were billed a certain amount. The ClearPath Medical Billing LLC Patient Help Desk service is designed to assist patients with any billing-related questions or concerns they may have.
The team at ClearPath handles inquiries from patients, explaining charges, clarifying insurance coverage, and guiding patients through any issues related to their bills. This service is incredibly valuable for healthcare providers, as it helps improve patient satisfaction, reduces confusion, and provides clear communication between the practice and the patient.
For example, if a patient has a question about their insurance coverage or the amount they need to pay, they can reach out to the help desk for assistance. This ensures that patients have the information they need and that billing issues don’t affect their relationship with the provider.
5. Account Receivable (AR) Services
One of the most critical aspects of medical billing is managing outstanding payments. When insurance companies or patients have unpaid bills, they need to be followed up on. ClearPath Medical Billing LLC provides comprehensive Accounts Receivable (AR) Services to make sure that all payments are collected efficiently and timely.
AR services involve managing the process of collecting money from insurance companies and patients. ClearPath’s team works diligently to follow up on unpaid claims, ensuring that providers receive the payments they are owed. They handle all aspects of accounts receivable, including:
- Tracking outstanding claims
- Sending reminders and follow-up communications to insurance companies or patients
- Resolving any issues or discrepancies that may be preventing payment
By outsourcing these services, healthcare providers can improve their cash flow and reduce the time it takes to get paid. This means fewer delays in payments and better financial health for the practice.
How These Services Benefit Your Practice?

When you partner with ClearPath Medical Billing LLC, you gain access to these critical services that help streamline your billing processes, improve your practice’s cash flow, and reduce the administrative burden on your team. Here’s how each service can make a real difference:
- Credentialing ensures you’re quickly approved by insurance companies so you can start accepting payments without unnecessary delays.
- Benefits Verification ensures you know exactly what’s covered by a patient’s insurance, preventing issues down the road.
- Claim Denial Management helps you deal with claim denials in an efficient manner, recovering payments that might otherwise be lost.
- Patient Help Desk improves communication with patients and clears up any confusion they may have about their bills.
- Account Receivable Services ensures you get paid promptly for the services you’ve provided, improving your practice’s financial stability.
By outsourcing these services, your practice can save time, reduce errors, and focus on what really matters: providing excellent patient care. ClearPath Medical Billing LLC makes sure the administrative side of your practice is handled professionally and efficiently, so you can spend more time helping patients and less time managing billing issues.
ClearPath Medical Billing LLC offers a comprehensive range of billing services designed to make the revenue cycle as smooth as possible for healthcare providers. From credentialing and benefits verification to claim denial management, patient support, and accounts receivable services, they provide everything you need to ensure your practice runs efficiently, gets paid on time, and maintains strong financial health
Outsourcing your medical billing can save your practice time, money, and stress. With benefits like fewer errors, faster payments, and more time spent with patients, it’s no wonder why many healthcare providers turn to professional billing companies. ClearPath Medical Billing LLC offers trusted, reliable, and expert billing services that can help you streamline your revenue cycle and improve your bottom line.

By partnering with ClearPath, you get access to an experienced team, competitive pricing, and a full range of billing services—all designed to support your practice’s success. If you’re ready to optimize your billing process and boost your revenue, ClearPath is the right choice for you.